In a proof-of-concept experiment, researchers successfully converted a pair of lungs into "universal" organs. In other words, in theory, these lungs could be transplanted into any recipient, regardless of blood type, as long as the organ size is appropriate.
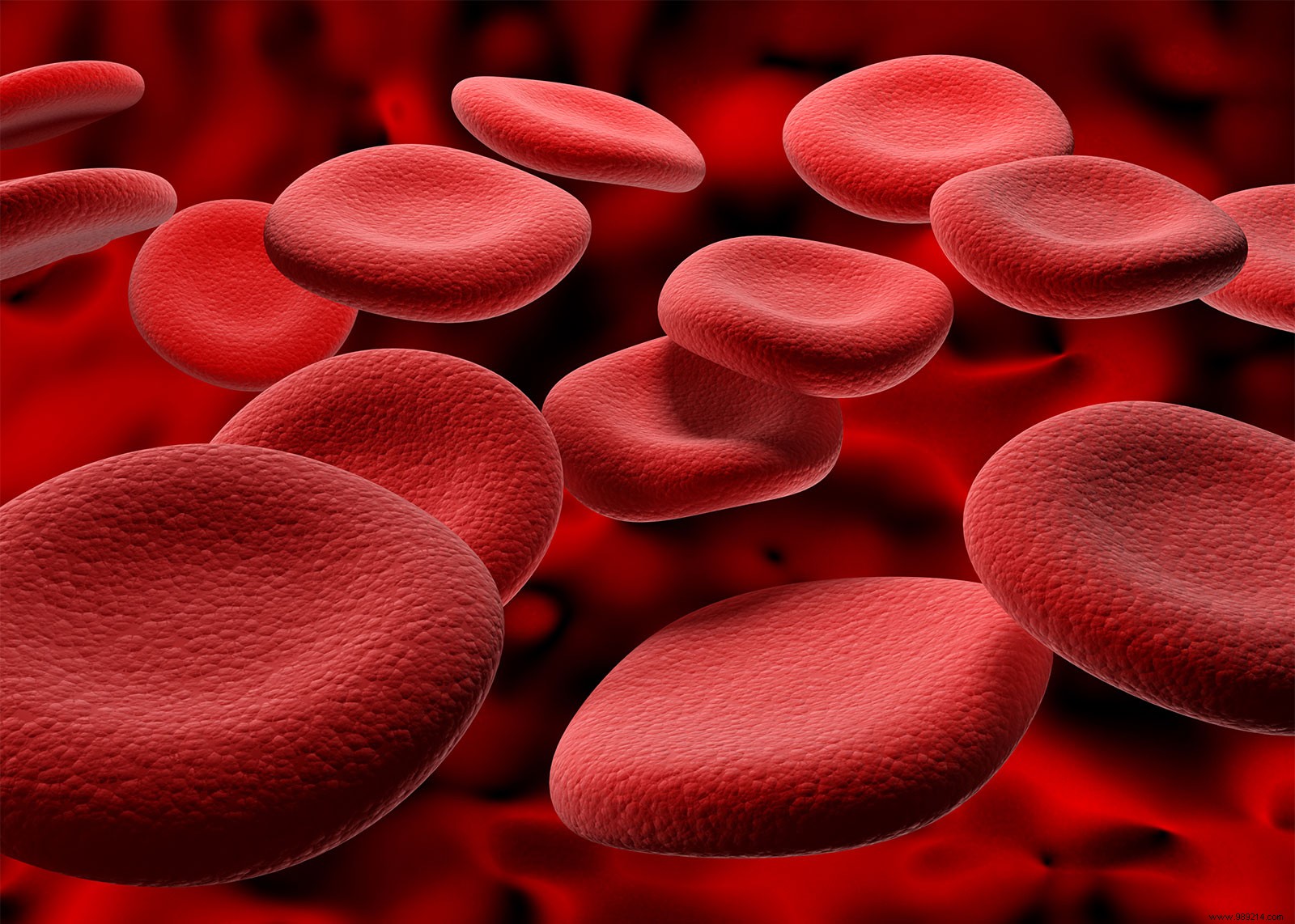
The different types of human blood are essentially distinguished by the combination of antigens that cover the surface of our red blood cells. Inherited from our parents, these antigens can be broken down into 35 broader blood groups, the most relevant being group A, B, O, depending on their rhesus.
More concretely, people with type A blood have only A antigens, while those with type B blood have only B antigens. people with type AB blood have both and people with type O blood have none.
While red blood cells carry these antigens, plasma contains antibodies that react to these antigens. Those with type A blood carry anti-B antibodies, for example. Thus, an individual "A" receiving a blood transfusion from a person "B" will have his immune system consider this blood as foreign .
Similarly, those with type O blood carry both anti-A and anti-B antibodies in their plasma. For this reason, type O organ recipients can only be matched with type O donors, who carry neither the A nor B antigens. On the other hand, because they are antigen-free, the Type O organs can be transplanted into any recipient.
So because these organs are in high demand, people with type O blood end up spending the most time on waiting lists. In fact, according to a study published three years ago, patients with blood type O have a20% higher risk of dying while waiting for a lung transplant than those of other blood groups.
To try to remedy this, Dr. Marcelo Cypel, surgical director of the Ajmera Transplant Center, and professor of surgery at the University of Toronto, has teamed up with Stephen Withers , from the University of British Columbia, with the goal of developing universal organs.
The latter's lab had worked in 2018 on a method to remove antigens from red blood cells A, B and AB to transform the cells into universal type O . The team had then discovered a group of enzymes in the human intestine capable of doing this .
In this new work, the researchers applied two enzymes, called FpGalNAc deacetylase and FpGalactosaminidase, to the lungs of donors with type A blood. These experiments were performed ex vivo (EVLP) in a machine capable of keeping the lungs alive outside the body for several hours.
The researchers then pointed out that by applying the enzymes for four hours, they could remove 97% of the A antigens from the lungs . Note that lungs can usually be stored in an EVLP device for four to five hours for lung transplants. The approach is therefore clinically applicable .
In another experiment, the team treated the right lungs of three type A pairs with the enzymes and left the left sides untreated. After four hours, she then perfused the organs with type O plasma which contains anti-A and anti-B antibodies and assessed the behavior of the different organs. Result:those treated with the enzyme worked perfectly well while the others soon showed signs of hyperacute rejection (massive congestion of antibodies that bind to the organ).

This new study therefore assumes that we could one day develop "universal" organs capable of fitting any recipient, provided of course that the size of the organs is appropriate . Eventually, this treatment could beused on a variety of other transplanted organs, as well as blood used for transfusions .
The next step will be to set up a clinical study. These trials on human patients will need to demonstrate that the enzymes used to remove blood antigens do not harm patients. We also know that at some point after the transplant procedure, the cells in the treated lungs will likely start producing blood antigens again, as the organ produces new cells. Would the immune system then suddenly attack the transplanted organ? This issue will also be investigated.